Analysis of COVID-19 and Telehealth Impact on Risk Adjustment
As COVID-19 continues to invade our personal and professional lives, every day brings new changes for the healthcare industry. Not long ago, health systems and provider organizations were instructed by the Centers for Medicare and Medicaid Services (CMS) to postpone, cancel or redirect any nonessential office visits, and even to limit in-person essential services, so that clinicians could focus critical resources and supplies on treating COVID-19 patients. This caused a significant disruption to the industry.
Almost a month after that announcement, CMS released guidance in response to the Guidelines for Opening Up America Again with recommendations for reopening facilities to provide nonemergent, non-COVID-19 healthcare. Still, despite an easing of restrictions, many providers are hesitant to reopen their doors and most patients are apprehensive towards going to a hospital or physician’s office for anything nonessential or nonemergent due to the risk of potential exposure to the virus.
In response to this environment, providers have turned to telemedicine as the alternative, and CMS has responded with increased flexibility and policy changes to ensure individuals receive the care they need without putting themselves or others at risk.
One area receiving attention is risk adjustment. Traditional strategies to close risk documentation gaps, such as in-home assessments and retrospective chart review campaigns, are no longer viable. In light of provider capacity constraints and the decline of nonessential services, health plans should reevaluate their risk adjustment programs and gap closure strategies to prevent revenue loss due to understated risk scores.
Telehealth Visits and Risk Adjustment
For the last several years, telehealth visits have been accepted for risk adjustment in the Affordable Care Act (ACA) market if they meet the appropriate criteria.
For Medicare Advantage (MA), CMS released an announcement on April 10, 2020, on the applicability of diagnoses from telehealth services for risk adjustment. According to the memo, MA organizations can submit diagnoses collected during telehealth visits as long as those visits meet the criteria for risk adjustment eligibility (i.e., allowable inpatient, outpatient or professional service, from a face-to-face encounter). This is valid for submissions to both the Risk Adjustment Processing System (RAPS) and the Encounter Data System (EDS).
What is the Impact of Increased Telehealth Flexibility?
Now that both MA and ACA plans have the “green light” for telehealth, you may be wondering “what’s next?”
There are a few probable outcomes of this major update:
- The shift to virtual care will lead to an increase in volume of telehealth visits that capture conditions used in risk adjustment reporting.
- Chronic conditions will be captured during inpatient visits at a higher rate than normal, especially because early indicators show that people with underlying health issues are at a higher risk for COVID-19.
- Essential visits will continue to decline as people follow state guidelines to shelter in place and avoid healthcare facilities unless faced with an urgent need.
- Critical essential visits will still be redirected to telehealth services, if possible, or other locations treating non-COVID-19 patients.
- Despite changes to site of care, top conditions will still be captured in 2020 as they require multiple provider visits to effectively manage.
- Health plans will need to explore other risk documentation gap closure strategies that do not rely on person-to-person contact and disruptive outreach.
To evaluate these hypotheses, we dive into the data.
Analysis of Risk Adjustment Impact
Using a proprietary dataset of 550,000 ACA lives from the Pareto Community, Pareto analyzed all scored claims with a documented HCC to identify the services, places of service and conditions that impact risk adjustment, in order to understand:
- Which services document the most conditions (i.e., HCCs) and how the volume of these services is affected by COVID-19
- Which locations of care are being most impacted by COVID-19
- Which condition categories capture the most HCCs, in which locations are these condition categories being documented, and how has that changed due to COVID-19
The analysis was conducted on claims from the Pareto Community in the ACA market for January to March 2020. For the results presented below, the data is limited to scored claims from the places of service most impacted by COVID-19: Telemedicine, Office, Hospital Outpatient Department - Off Campus (HOPS-OFF CAMPUS), Hospital Outpatient Department - On Campus (HOPD-ON CAMPUS), Hospital - Inpatient (HSOP-INPATIENT) and Ambulatory Surgery Center (ASC).
Which services document the most conditions?
The chart below demonstrates the services that have historically captured the most chronic conditions.
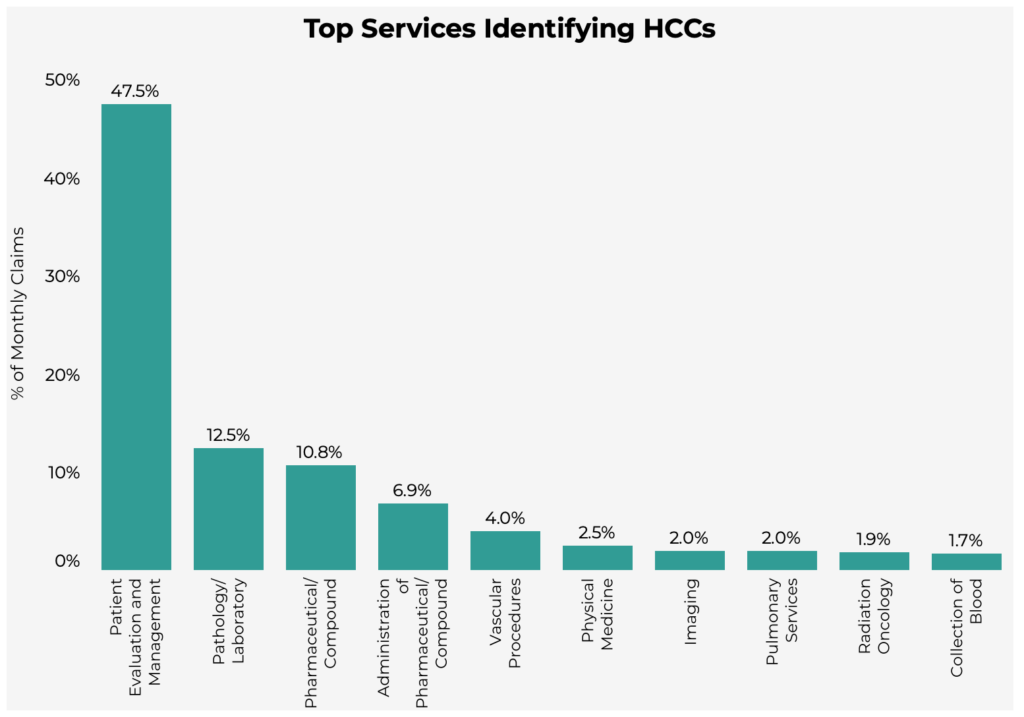
"Patient Evaluation & Management" services accounted for 47.5% of HCCs across all places of service. Health plans should consider redirecting these services to telehealth whenever possible, in order to ensure all relevant diagnoses are evaluated and documented.
Has COVID-19 impacted the volume of these services?
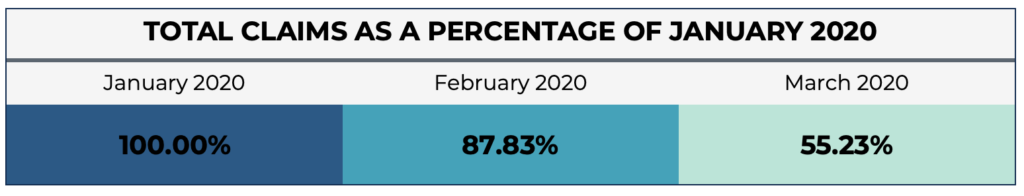
Across the board, all services and procedures are being impacted by COVID-19. The table below demonstrates the reduction in volume as a percentage of January claims for the top 10 services that have historically captured the most chronic conditions.
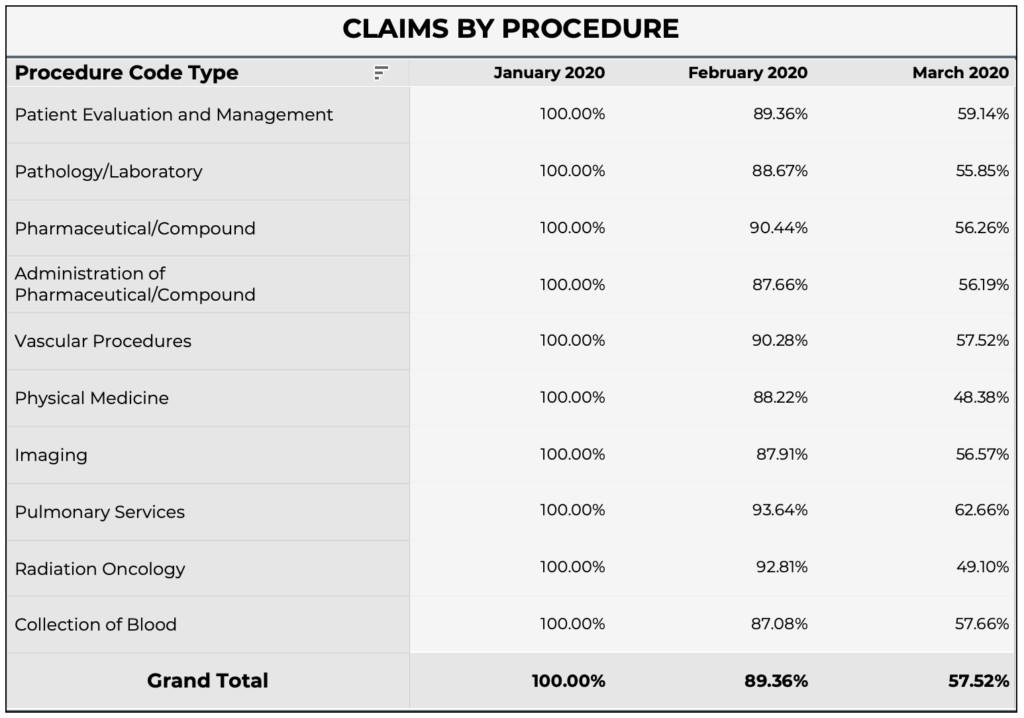
As expected, the amount of “Patient Evaluation & Management” services have been nearly cut in half, with only 59.1% of January claims volume in March.
Other services, such as “Radiation Oncology” and “Physical Medicine (PT/OT),” have dropped even further in March to 49.1% and 48.4% of January claims volume, respectively.
Because the most risk-adjustable conditions are documented through these services, and they are being performed less often, health plans will likely see a significant increase in undocumented risk gaps—until the diagnoses that would normally be documented through these services are documented elsewhere or through gap closure initiatives.
Which locations of care have been most impacted by COVID-19?
In addition to a decline in services performed, the locations people are visiting most often for these services are changing dramatically.
The graph below sorts claims by place of service, and using January as a reference, demonstrates the change in volume by month.
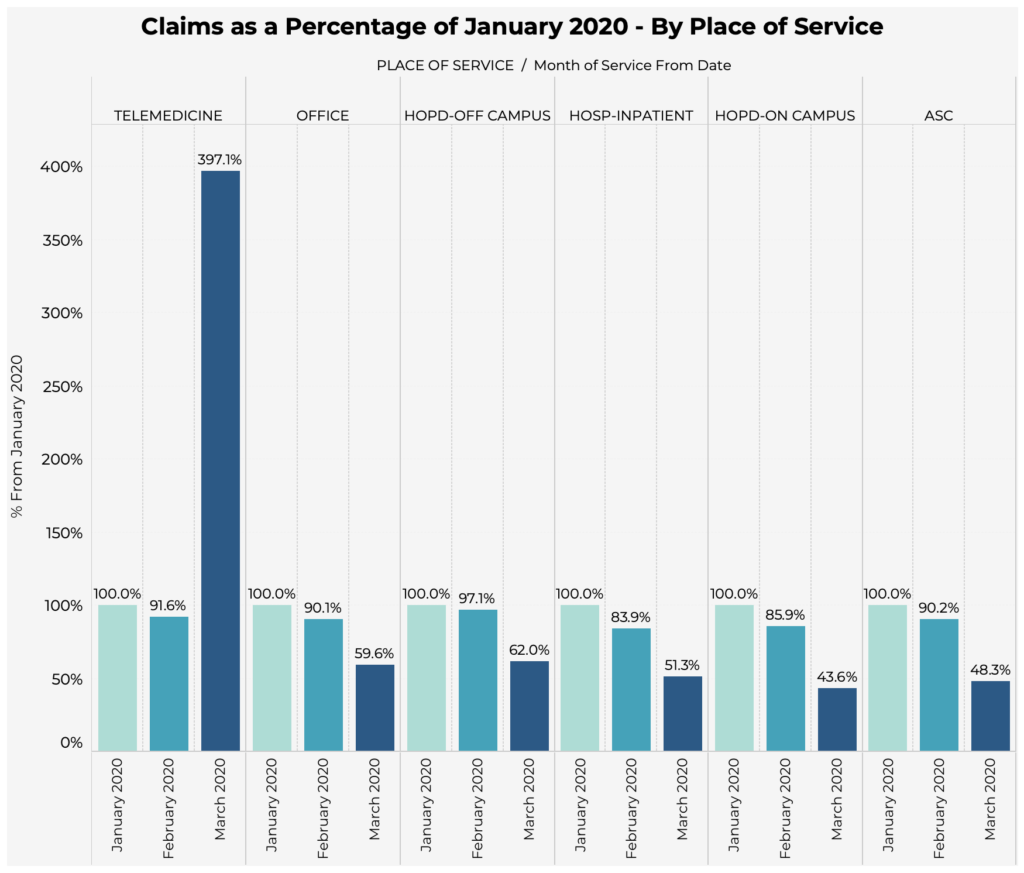
The most significant shifts occurred in March. “Telemedicine” visits increased 397% compared to January volume, whereas visits to “Hospital Outpatient Departments – On Campus” have decreased to only 43.6% of January volume.
With less visits to in-person sites of care, health plans can no longer rely on these locations and the services performed there to capture conditions with a risk adjustment impact. Plans have already begun enhancing telehealth programs and activating new risk adjustment strategies (e.g., virtual in-home assessments); we anticipate seeing increased use of telehealth to evaluate and document diagnoses. Plans should also expect to see more conditions documented in different or atypical locations, such as “Hospital – Inpatient” visits, as people refrain from seeking care unless absolutely necessary.
What are the top condition categories captured in claims data?
Below are the top 10 condition “groups” or categories capturing the most HCCs across all places of service.
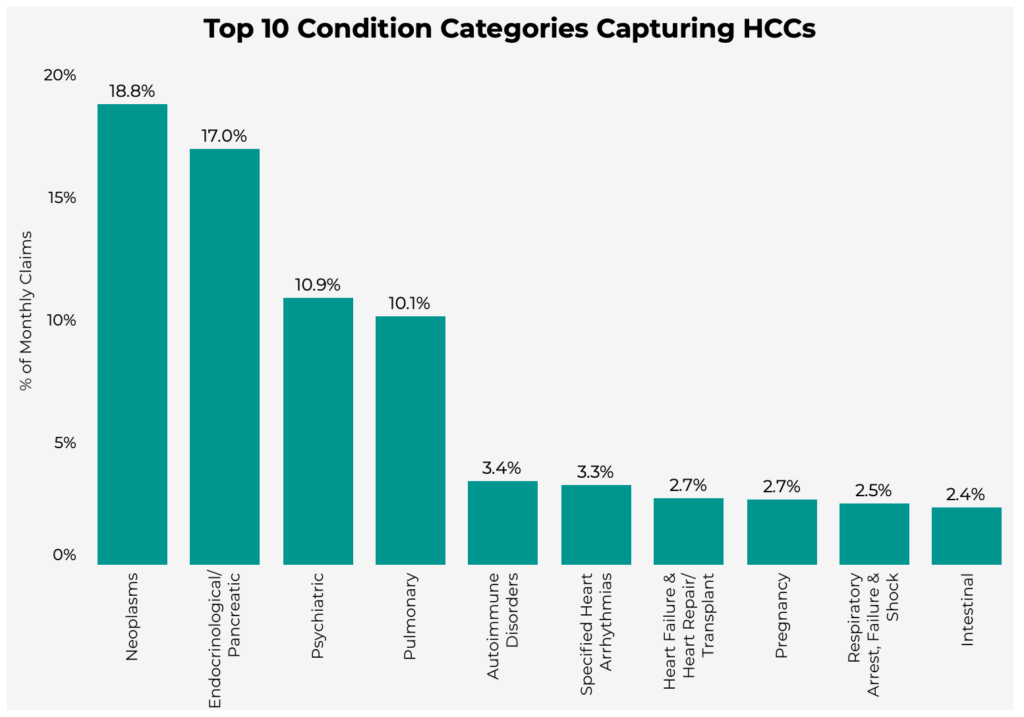
The analysis shows that "Neoplasms" have the most associated HCCs. When combined with the places of service in which these conditions are documented (shown in the following section), health plans can identify where gaps may exist within their specific population and use this information to target member segments for risk adjustment.
How has COVID-19 impacted the capture of HCCs at affected places of service?
While overall volume of services and procedures is decreasing, diagnoses are still being captured via other places of service, such as telemedicine.
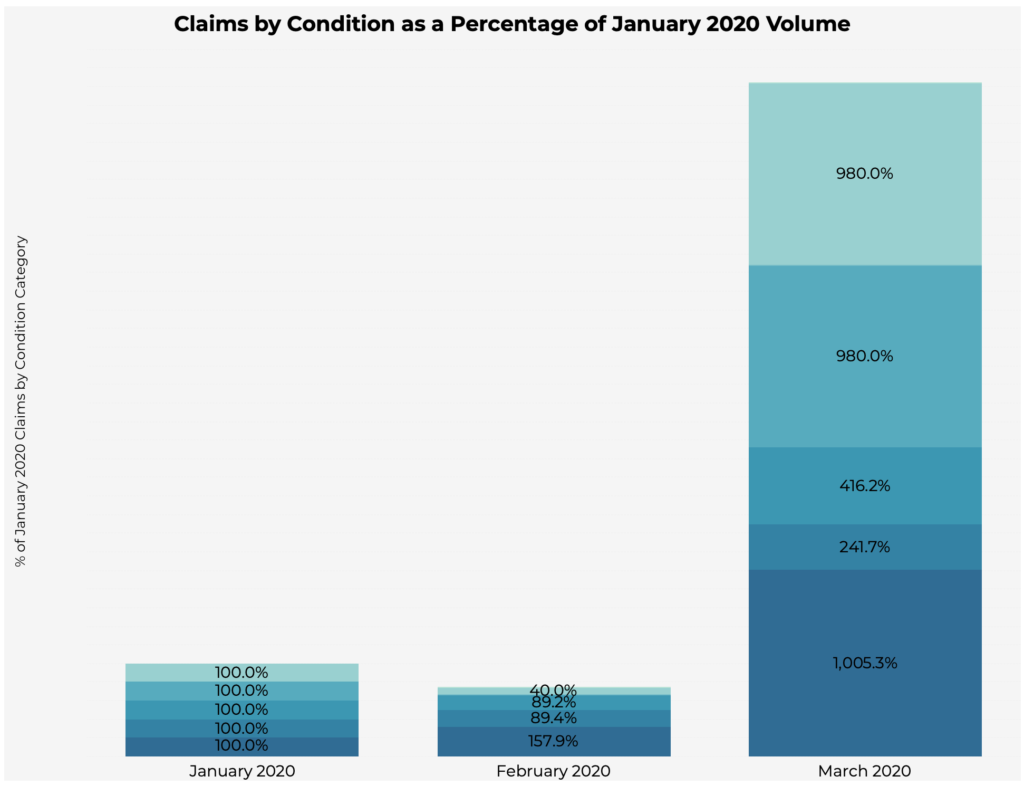
Since January, “Telemedicine” visits for Pulmonary conditions increased by 1000%, while “Hospital Outpatient Departments – Off Campus” visits reduced to 42% of January claims volume. “Telemedicine” visits also increased by nearly 1000% for Neoplasms & Endocrinological/Pancreatic conditions.
While overall volume of services is decreasing, there has been a rapid rise in the use of virtual visits to capture a broader array of HCCs. It's unclear how long the impacts of COVID-19 will last, but expect to see more health plans adding telehealth to risk adjustment program strategies as an ongoing solution, beyond addressing the challenges of this pandemic environment.
Conclusion
Using this analysis as a baseline, Pareto will continue to record data monthly through 2020 to gain additional insights that may impact risk scores. A live version of this report is available here.

The above insights are based on a general ACA population; however, Pareto can run this model using plan-specific data to establish targeting from a defined population in MA or ACA. When combined with our COVID-19 risk model, which identifies the individuals in your membership with a high risk of severe complications from exposure to COVID-19, we can help you prioritize the members to target for communication, intervention and more. Contact us for more information.
