The Last Puzzle Piece: Final Risk Adjustment Coefficients for 2018
The Department of Health and Human Services (“HHS”) recently released the much anticipated Final Risk Adjustment Model Coefficients for the 2018 Benefit Year. This updated report finalizes the risk coefficients for demographics, diagnosis codes (hierarchical condition category [“HCC”]), prescription drug class (“RXC”), and HCC + RXC interactions that were published as draft in the 2018 Notice of Benefit & Payment Parameters (“NBPP”) rule released late last year. Using the updated coefficients, Pareto conducted an analysis of year-over-year changes to the risk adjustment model, specifically from 2016, 2017, 2018 draft model, and 2018 final model. The results of this analysis are summarized below. Each HHS model was analyzed by applying it to the same 2016 dates of service membership and claims experience from across the Pareto community.
Key Takeaways from the 2018 Final Rule
Many of the themes outlined below are consistent with the changes discussed in a previous alert on the draft 2018 NBPP. The estimated quantification of the impact, however, becomes clearer with the finalized risk coefficients. While the actual impact will vary greatly between plans based on their unique risk makeup, the information below provides general guidance for what to expect in the coming year.
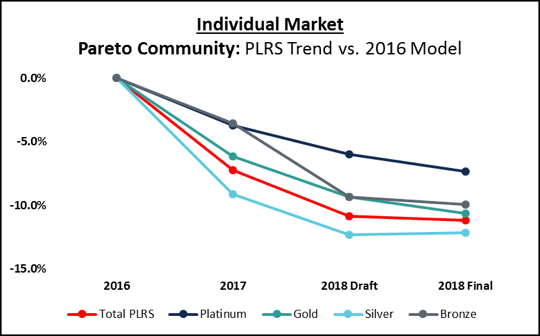
- Lower Overall PLRS – As HHS continues to inch towards a 1.000 average Plan Liability Risk Score (“PLRS”), expect to see, in general, a decrease in overall health plan PLRS. For frame of reference, our analysis has shown a 12% overall PLRS decrease for the Pareto community from the 2016 model to 2018 final model. This trend is consistent for both the Individual and Small Group markets, but the change by metal level is much more variable in the Individual market, with bronze metal members impacted the least.

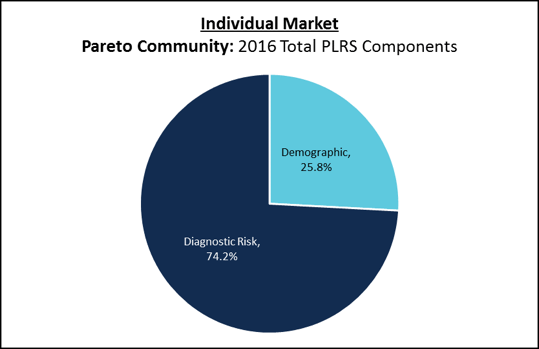
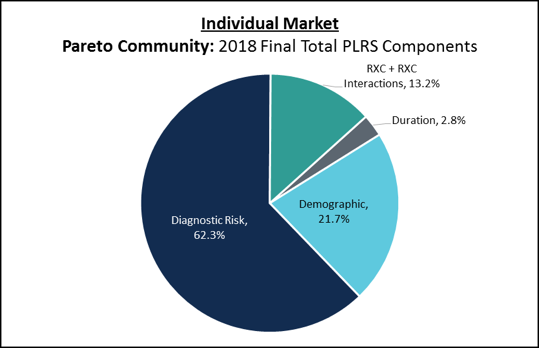
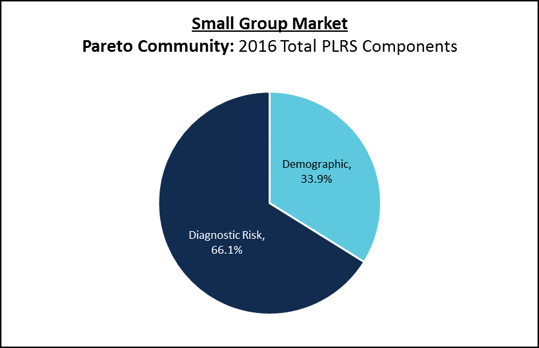
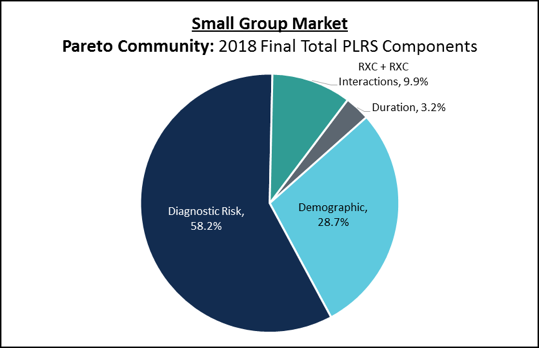
- Shift in PLRS Makeup – When we look at the components of PLRS, what used to be an approximate 70/30 split of diagnostic risk and demographic risk is now much more complex. Diagnostic risk as a total of overall PLRS has reduced 8-12%, while additional risk factors have been incorporated to offset this reduction: Duration Adjustment Factor (“DAF”), RXC factor, and interactions for HCCs with a correlated RXC. The charts below demonstrate this rebalance of risk makeup from the 2016 model to the 2018 model in both the Individual and Small Group Markets.
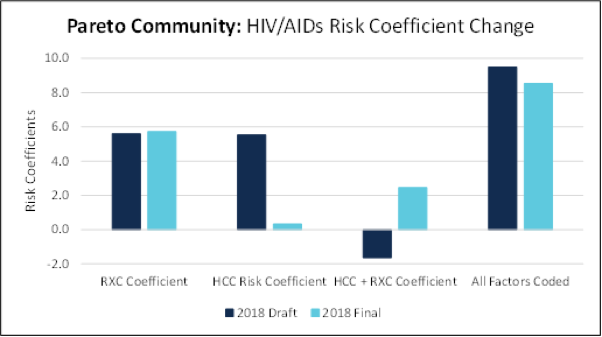
- New Risk Factors – The addition of pharmacy data to a member’s risk score is the most significant change from the 2017 model to the 2018 model, as it adds two new factors to risk calculations: drug or RXC and the interaction of capturing both the diagnosis and RXC. With 2018 being the first year for incorporating drug data into the risk adjustment model, HHS made some significant changes to the risk coefficient distribution between HCCs and their corresponding RXC. The changes are HCC / RXC specific and will impact plans differently based on their diagnostic coding performance and the proportion of members managed with one of the associated prescription drugs.Highlighting HIV/AIDS below, the majority of members with the condition were both documented and had a correlated prescription. The 25% that only had the HCC documented or the prescription are impacted by the change in risk coefficients made between the 2018 draft and 2018 final. HHS significantly reduced the HCC risk coefficient and increased the interaction factor, placing greater emphasis on capturing both components.

Note: The above exhibits are limited to the Individual Market.
So What Can Plans Do?
Evaluate the Impact of Your Risk Score: Plans should expect overall PLRS to continue to fall (holding population mix constant), but by how much is dependent on the unique makeup of each health plan’s population relative to the market. Plans should evaluate the impact to their population, and to the extent they have market transparency, evaluate whether these model changes increase or decrease plan PLRS relative to the market.
Focus on Prospective Documentation Capture Efforts: The medical record is the ultimate source of truth for risk documentation, so plans should continue to evolve their Revenue Management strategies to focus efforts on achieving complete and accurate documentation at point of care.
Prioritize Efforts Based on the Recent RA Model: Though this Alert focuses on the 2018 RA model changes, significant changes were made to the 2017 model impacting individual HCC risk weights. Plans should assess these changes for guidance on prioritizing prospective and retrospective campaign efforts. In preparing for 2018, the inclusion of RXC will significantly impact the prioritization of those impacted HCCs, and factoring in whether the RXC has been captured will impact plan prioritization.
Evolve Retention & Acquisition Strategies: Changes to the risk model alter the definition of those members and conditions a health plan effectively manages. These changes should be proactively assessed and incorporated into a guided sales and market strategy.
