CMS Announces an EDS Reporting Extension
On October 20th, the Centers for Medicare and Medicaid Services (“CMS”) informed Medicare Advantage Organizations (“MAOs”) that the encounter data submission deadline has been extended for the second final reconciliation of Payment Year (“PY”) 2016 to April 2, 2018. This allows MAOs to reevaluate their Encounter Data System (“EDS”) submissions and correct any unreported information to improve risk score accuracy. This memo did not adjust the Risk Adjustment Processing System (“RAPS”) submission deadline, which was January 31, 2017.
Data Quality Issues
EDS only accounts for 10% of an MAOs total risk score for PY2016, and though a minority share, data quality issues can still have a material financial impact. Our experience has shown that MAOs typically have a 1-3% data quality issue, translating to $5M-$15M in premium shortfall for a 50,000 member plan ($500K-$1.5M for EDS alone at 10% of overall risk). The extension provides MAOs with an opportunity to evaluate their end-to-end data process to ensure the completeness and accuracy of their submissions.
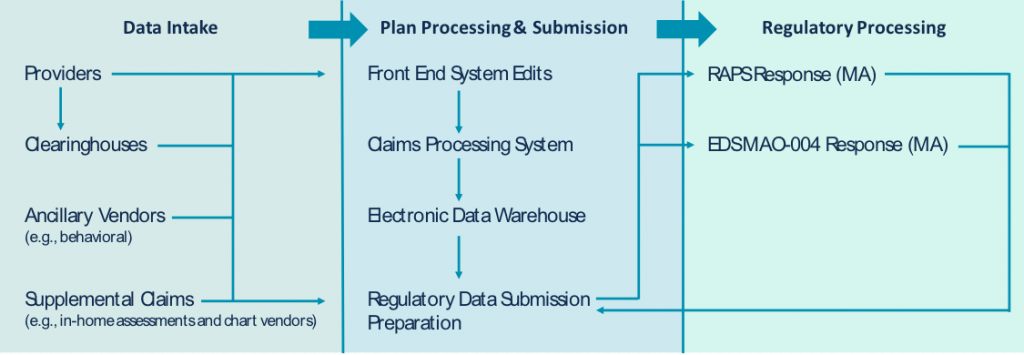
Through our work assessing plans’ end-to-end data integrity for both Medicare Advantage (“MA”) and the Affordable Care Act (“ACA”) markets, we’ve uncovered that 65-80% of all data quality issues exist prior to submission. Many MAOs primarily focus on their acceptance rates and error remediation, missing the fact that not all information has been submitted in the first place. As illustrated below, the disparate nature of the information collected by MAOs paired with the multiple systems and data transfers involved create an environment where it’s difficult to know whether all relevant information has been submitted to and accepted by CMS.
What can MAOs do?
Complete an end-to-end data integrity assessment. Evaluating end-to-end data integrity ensures that all information received (e.g., billing 837s, supplemental records from chart reviews, etc.) is making it through to submission and acceptance by CMS without any degradation. Obtaining data extracts from each point of the data process may be administratively taxing, so assess data availability and complete the evaluation in stages, if necessary. Just evaluating whether all post-adjusted claims data is being submitted and accepted can uncover significant improvement opportunities.
Root cause investigation to prioritize remediation. Step one is determining where in the process data quality issues have occurred. Step two is figuring out why. Root cause investigation can be time consuming; therefore, applying advanced data science and analytics can cluster encounters around common themes (e.g., diagnosis truncation, particular claims types, etc.) to expedite root cause investigation and remediation efforts.
Establish ongoing quality controls. Internal systems and regulatory reporting requirements are continually changing. It’s critical to have proven quality controls in place to ensure the completeness and accuracy of ongoing submissions. Adequate quality controls evaluate the integrity of a MAOs data throughout the end-to-end process and not just on the submission & error resolution phase of the process, while providing timely and actionable insights to correct issues before report deadlines.
